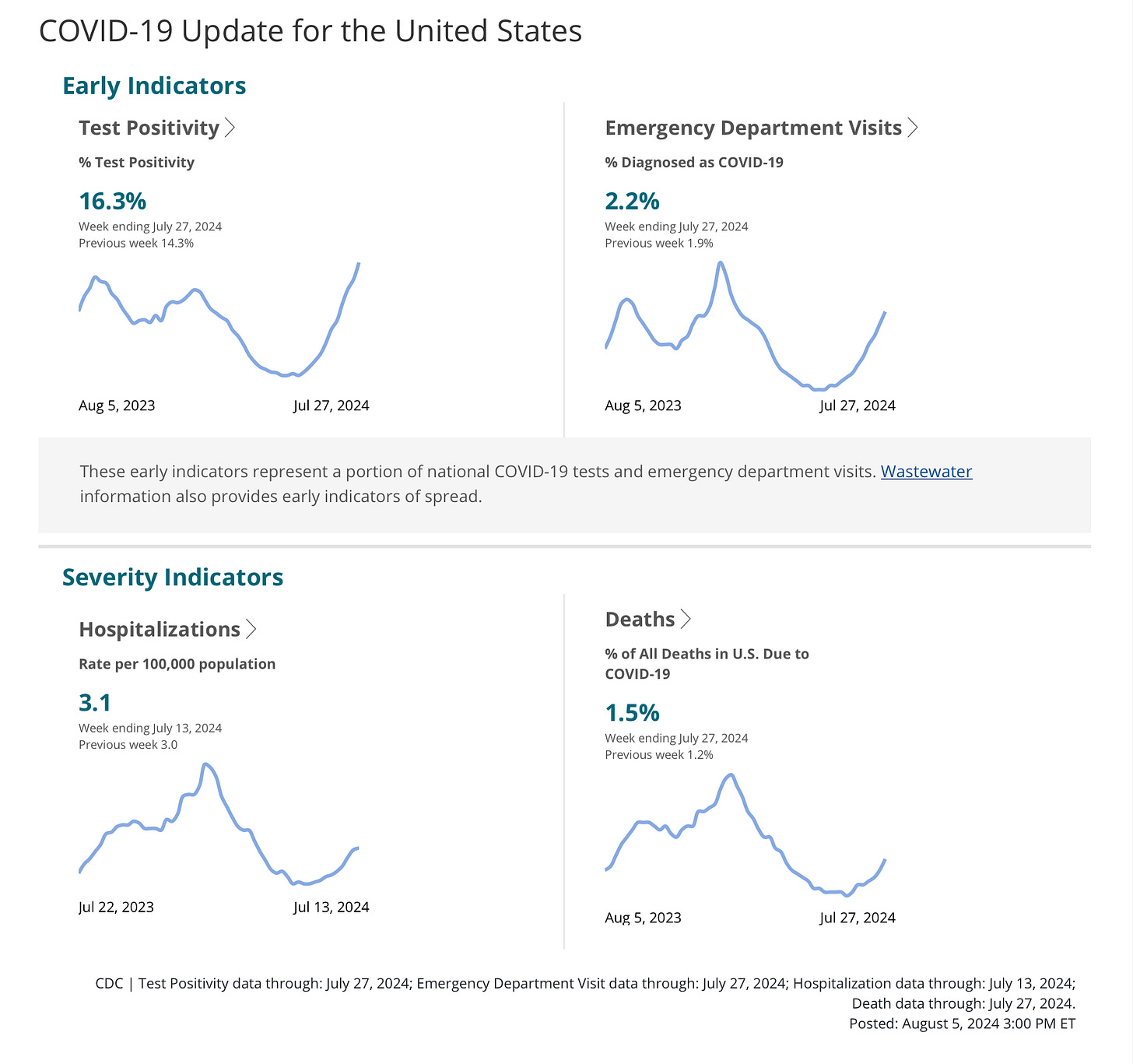
I’m going to spend some time discussing COVID for a change—if you’d rather not bother, skip ahead and there might be a topic further on to interest you. Your recent impression that everywhere you turn people are coming down with COVID again is correct—this summer wave is more intense than last summer, and shows no signs of letting up. In addition to continuing to have twice yearly peaks, instead of the usual respiratory virus pattern of a single cold weather surge, the SARS2 virus once again is showing off its resilience and astonishing ability to rapidly evolve and outwit our immune defenses. The epidemic (can’t call it a Pandemic anymore since that was declared over a long time ago by someone with a higher pay grade than me) is particularly acute in the western US, with California having some the highest levels. The familiar CDC charts below show the continuing increase in the test positivity rate, currently impressively high at 16%, and the continued rise in the percent of emergency room visits due to COVID.
The situation in California reveals that by every metric the amount of COVID disease is far greater this summer than last, and the amount of virus circulating in the waste water is rivaling the kind of levels seen at the height of the 2023 winter surge. Follow the dashed grey line in this graph to see that overall US viral burden has passed the 2023 summer peak, and the solid line tracing California is close to DOUBLE that. LA county hospitalizations (which they are still reporting as actual numbers) are averaging almost 400/day, which is about 2/3 of last year’s peak.
Here we are four and a half years into COVID and the virus refuses to behave in any predictable way. The current recent top dog variant KP.3.1.1 came on very strongly from early June, when it was only 1-2% of viral sequences, to now 27%. Although it differs from the closely related KP.2 and KP.3 by very small structural differences in the spike protein, this rapid replacement of the other strains, coupled with the marked summer increase in community viral burden, shows that those changes are sufficient to elude prior immunity against infection. For generally healthy and younger folks our combined natural immunity from multiple infections and vaccination remains sufficient to prevent critical disease; as usual though, the very elderly and medically unwell have no such guarantee.
If you are essentially ignoring COVID because you believe that disease severity for the average person has decreased over time, that would be a fairly understandable assumption, but it might not be correct. A recent study from the NIH found that the severity of a prior episode of infection was strongly linked to the severity of subsequent infections.
Hadley, E., Yoo, Y.J., Patel, S. et al. Insights from an N3C RECOVER EHR-based cohort study characterizing SARS-CoV-2 reinfections and Long COVID. Commun Med 4, 129 (2024). https://doi.org/10.1038/s43856-024-00539-2
We know now that around 40% of COVID infections may be asymptomatic, and the data from the current NIH study found 87% of people reporting a first infection had mild disease not requiring any medical attention. A more accurate view of things seems to be that this disease was always very mild for the vast majority of people getting infected—but if you had a serious case of COVID the first time around, you are at fairly high risk of a repeat experience. You could use this information to make an assessment of whether you should make alterations in behavior during periods of high disease activity—or you could just ignore the whole situation, go to that Taylor Swift concert or Dead and Company at the Sphere, and enjoy yourself. The vaccine horizon is following the unfortunate but predictable path of the last three years. The new vaccine will target the KP.2 variant (if you opt for the Novavax shot it will be JN.1) and of course that mutant will be completely replaced by the surging KP.3.1.1 variant by the time the vaccine is available. Despite this, we can predict with a good deal of certainty that a booster dose of vaccine will temporarily increase your protection from severe disease, if you are in the group needing that. We can also predict that it will have only moderate efficacy in preventing infection, and only for a couple of short months.
A month ago I discussed the exploding epidemic of Mpox (monkey pox) spreading over the past year in Congo, and predicted it would soon reach out to surrounding African nations. This is happening sooner rather than later, as you can read in the following article from Science. Just to review briefly, the virus causing this huge outbreak is the more deadly Congo clade I Mpox, which has acquired the ability to spread easily via sexual contact, and currently has a mortality rate of 3%, with severe morbidity for many surviving people. The two most efficient ways for a virus to spread among the human population are via the respiratory route, or through physical contact, especially sex. No, Mpox won’t be the next HIV like pandemic for a couple of key reasons. There is no prolonged chronic infectious state, where asymptomatic people can go about spreading the virus to many other individuals for years. While infected people may be able to shed the virus for a very brief time before they become symptomatic, once symptoms begin they are fairly recognizable and avoidable. Because the disease is acute, and people either die or recover in three to four weeks, there will not be an ever increasing number of infected people with a life long disease. Finally, there is already a moderately effective Mpox vaccine, and a good road map toward perhaps improving on this in a relatively short time; whereas 44 years into the HIV pandemic there still is no vaccine. Nonetheless, given conditions in Africa, I expect the epidemic to spread and worsen significantly there, with some spill-over to the more developed nations.
Deadlier strain of mpox spreads to multiple African countries | Science | AAAS https://www.science.org/content/article/deadlier-strain-mpox-spreads-more-african-countries
In a recent post I mentioned that we humans carry the remains of ancient retroviruses which intercalated their genomes into our DNA millions of years ago. It’s been known for many years that certain viruses which we acquire during life have the ability to cause cancer: Hepatitis B with liver cancer, human papilloma virus HPV with cervical and oropharyngeal cancer, Human Herpes Virus 8 with Kaposi’s Sarcoma, and EBV Epstein-Barr virus with nasopharyngeal carcinoma. There is more recent evidence that the ancient retroviruses in our DNA, which are no longer capable of causing productive viral infection, have the potential to act as tumor promoting factors. Cancer is generally not a single switch which is either off or on; cells follow a trajectory where some initial insult triggers a progressive cascade of events which are self-reinforcing, taking the cell further and further along a pathway to dysregulated and then uncontrolled growth. These primate specific endogenous retrovirus sequences (ERVs) in our genome can be activated by certain oncogenic signals in the early stages of malignant transformation, and then contribute to an ever widening web of abnormal gene activation and progressively more bizarre cellular functioning. I’ll put a link to the the recent article, in Science Advances, but it is for experts in the field (which I am not). The bottom line is we are learning that viruses negatively affect us in ways we couldn’t have even imagined a few decades ago—and you now can blame some ancestral life form eons ago for bad genetic baggage, and cut your parents and grandparents some slack.
Endogenous retroviruses mediate transcriptional rewiring in response to oncogenic signaling in colorectal cancer | Science Advances https://www.science.org/doi/10.1126/sciadv.ado1218
The final item for this week highlights the increasing need for American doctors to become adept at diagnosing and treating diseases they never encountered previously in the US. I mentioned this a long time ago, as a consequence of the uncontrolled migrant surge into the country, coinciding with fewer physicians pursuing advanced training in Infectious Diseases. It is frequently apparent to a doctor that their patient has an infectious disease, and if the specific diagnosis or treatment is obscure, then it’s also obvious where to call for help. The following article is a wake up call since it alerts us to just how common a life threatening, late, complication of an occult infection acquired years ago may be in this migrant population. Chagas disease is an endemic infection throughout Latin America and Mexico, transmitted by the bite of the common reduvid bug. The acute infection is a mild, self-limiting affair (rarely diagnosed), but the organism establishes a chronic infection in 20% to 30% of people, and years later can cause cardiac and esophageal damage, with congestive heart failure the most severe consequence. This is estimated to be the most common cause of pacemaker placement in Brazil. The following paper details how frequent late, untreated Chagas disease may be as a cause for cardiac pathology in this population. This report from a DC hospital system looked at all patients referred for an echocardiogram, and found that 16.7% of people from regions endemic for Chagas Disease had evidence of prior infection. When the lens was narrowed to patients presenting with congestive heart failure, the rate of prior Chagas infection rose to 25%, and when they looked at patients referred for a cardiac electric conduction defect called bundle branch block the incidence was 31%. The American Heart Association estimates that given the recent influx of 11 to 12 million migrants, with the vast majority coming from regions where the disease is endemic, there may be as many as 300,000 people now in the US with previous Chagas infection.
: Kerai A, Ritika Gadodia R, Aberra T, et al.: Seroprevalence of Chagas cardiomyopathy among hospitalized Latin American immigrants within a Washington, DC, hospital. JCAA Heart Failure 2024; DOI: 10.1016/j.jchf.2024.05.025.
Watching the Olympics these past 2 weeks has taught me some important lessons. Even though you might be writing about a completely fascinating subject like Infectious Diseases, you shouldn’t try and compete for attention with the best athletes in the world. It’s unwise to swim in the river of a city with a medieval sewer system—no matter how much money the politicians claim they have spent “cleaning it up”. If you are a woman, and you are competing in a setting where the enlightened powers that be dictate you must compete against individuals harboring a Y chromosome, I recommend you choose badminton, marksmanship or women’s gymnastics, rather than boxing. No matter how hard your XY opponent hits the shuttlecock, it is unlikely to permanently maim you. The XY competitors never show up for balance beam or uneven bars for some reason; and with competitive shooting you have a ready means to defend yourself against that toxic testosterone nonsense. Finally, if you are looking for accolades about your production from the world’s top athletes, don’t put them up in cardboard beds, feed them meatless meals (unless requested), and do give them air-conditioning in the summer. If you find these posts informative, then you know what to do with the like button at the top.





Always enjoy reading your current events comments. Funny but so true.