COVID Upswing the Asia
The tangled world of Polio vaccine.
While most of the world continues to have decreasing numbers of COVID cases, there are some concerning hotspots, especially in the far east. We know there is a massive wave of COVID washing through China right now, with very little timely data being collected or shared. That’s understandable, the authoritarian regime there was forced to end its zero COVID policy, or risk an uprising, and the way to save face was to pretend the problem was “conquered”. So no more lockdowns, no more mass testing, no reporting of hospitalizations or deaths—what you don’t see isn’t real, like Uyghurs in detention camps (sorry I meant re-education centers), or the chaos at our own southern border. Australia, a place that’s freely sharing data that I would bet a nice barby on its accuracy, is also bucking the world wide trend. It’s too early for them to be having a “standard Winter wave”, but cases there have been increasing for months, doubling from an early March low, and up 28% from April. This fifth wave of COVID in Australia is different than previous waves, it has been building slowly and steadily but with much lower case counts than previous surges. How much of that difference is due to accumulated immunity versus the decline in testing is hard to know. Deaths also have been on a steady slow upslope since sometime in late March. It’s not an Omicron tsunami, but unexpected now that the Pandemic is over, and the virus is supposed to play by the polite endemic rules. The Public Health authorities in Australia are suggesting it’s because a very sizable chunk of the population passed on the last vaccine booster dose—perhaps, but the same is true in the US and other locales where disease and death have continued on a downward course. It’s a complex question involving population demographics, timing and variant composition of prior waves, vaccination schedules, and many other variables. Various people with letters after their name will always be happy to pretend they have the answer, if you will just listen. Masks in Aussie healthcare facilities are no longer required, unless you’re a healthcare provider taking care of a COVID patient; and the the virus apparently has taken note, causing the nosocomial spread in one Canberra hospital to 12 patients and 5 staff members. People hospitalized for some other serious condition are the last people you want to spread COVID to. Following is a graph of weekly deaths down under, note the slope trending in the wrong direction.
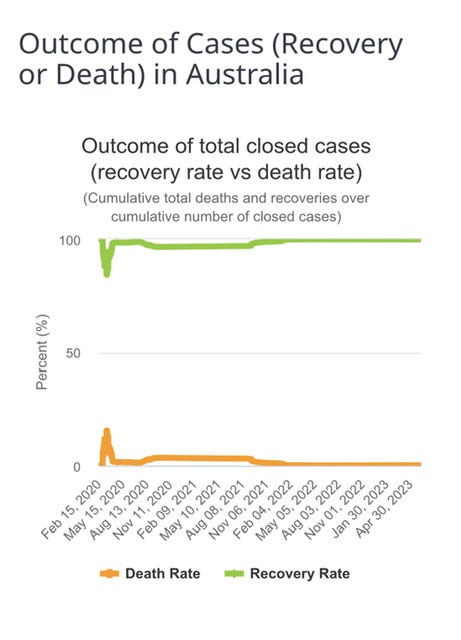
Here is another interesting graph from down under. It shows the case fatality rate since the start of the pandemic. This has nothing to do with the number of cases, just the outcome of cases. Notice the extremely high mortality rate in the first wave, which rapidly decreases prior to the availability of vaccines, monoclonal antibodies, convalescent serum or antivirals. Australia shut down very quickly with travel bans and lockdowns and this was not a result of the healthcare system collapsing under an avalanche of cases. I interpret it as most likely representing a brief period of a learning curve; with doctors confronting a new disease with a variety of unknown characteristics and complications, and then quickly figuring out how to manage it optimally with the usual tools at hand. I suppose an alternative explanation might be that people were told, “Don’t come to the hospital unless you’re turning blue and want the ventilator”. I have no idea if Aussies received that New York message, but I prefer the first explanation.
In case you would factor viral activity into your vacation plans, here are the other destinations in the far east region with the highest proportional increases in recent COVID cases: China, Japan, Mongolia, Cambodia, Laos. Perhaps you’re looking to stay in this hemisphere where the COVID curve looks favorable—just be aware that Peru is experiencing their worst seasonal epidemic of dengue on record, with over 200,000 cases and 200 deaths so far. There is no vaccine or specific treatment for dengue, so speak to your travel agent. People at highest risk for severe Dengue Fever or death are those who have had the infection before; unlike COVID, prior immunity can work against you with this mosquito transmitted disease. That has been the major impediment to finding an effective, safe vaccine. Here is a current dengue ward in Peru—it’s recommended to bring your own mosquito net.
Finally today I’d like to return to the issue of oral polio vaccination, discussed previously in “What’s Wrong with the Vaccine World”, on 3/25. If you’re not familiar with circulating vaccine related Polio, that post will provide background. Wild-type Polio virus was eradicated from North and South America 25 years ago. The natural disease was declared eradicated in Africa five years ago. There has been one case of Wild-type polio (WTPV1) on the continent this year, in Malawi, which appears to have been imported from Pakistan, one of the only two remaining countries where the natural disease still exists. Of the three strains of Polio, types 2 and 3 are felt to be extinct, with only type 1 still causing natural cases. So far this year there have been four cases of WTPV1 in Afghanistan—the last case of paralysis occurring in a child who had received the regular three primary doses of oral polio vaccine, and then four more doses during follow up vaccination drives. While OPV performs well in wealthy first world settings, it has been recognized for years that its efficacy in tropical and poor nations is much lower, in the range of 70% or less. One study from northern India found seroconversion (meaning protective antibody levels) to type 1 Polio of only 12% following one dose of vaccine. This is variously attributed to malnutrition, enteric co-infections interfering, and a poorly defined entity, let’s call it “third world enteropathy”.\
Grassly NC, et al. New strategies for the elimination of polio from
India. Science 2006; 314: 1150-1153).
Against this background of minimal natural cases occurring in only two countries, contrast that with the number of cases of paralytic Polio due the oral vaccine (cVDPV, circulating vaccine derived Polio). The information following is taken from the WHO and CDC.
4). During 2021–2022, there were 88 active cVDPV outbreaks, including 76 (86%) caused by cVDPV2. cVDPV outbreaks affected 46 countries, 17 (37%) of which reported their first post-switch cVDPV2 outbreak. (further clarified below). The total number of paralytic cVDPV cases during 2020–2022 decreased by 36%, from 1,117 to 715; however, the proportion of all cVDPV cases that were caused by cVDPV type 1 (cVDPV1) increased from 3% in 2020 to 18% in 2022, including the occurrence of co-circulating cVDPV1 and cVDPV2 outbreaks in two countries.
The next time someone tells you very authoritatively that there has never been a laboratory created virus freely circulating in humans and causing serious disease, refer them here. Now there is a little complicated background, so bear with me. Some years ago it was recognized that the type 2 virus in the oral vaccine was causing almost all of the outbreaks of paralytic Polio due to circulating vaccine virus (cVDPV2); and after type 2 virus was declared extinct, the oral vaccine was changed world wide in 2016 to include only types 1 and 3. So how are we still having outbreaks of vaccine derived Polio 2 this many years down the road? The answer is the vaccine strain 2, which “reverted” to a neurovirulant form, has been in chains of circulation within communities around the world. Now of course we are beginning to see more outbreaks of cVDPV1 as the cause of paralytic disease, but cVDPV2 is still by far the biggest culprit. Recognizing the magnitude (not to mention the bad PR) of the problem, the vaccine scientists set out to make a novel, safer type 2 Polio vaccine strain (nOPV2), which became available just over a year ago in 2021. Prior to that, you need to know that every time there was an outbreak of type 2 vaccine related Polio (or emergency as the WHO refers to it) the response would be to rush into the area and give out more of the same vaccine which had caused the problem in the first place. Although this approach might seem counter-intuitive, it’s not quite the same as using gasoline to put out a grease fire in the hopes of using up all the available oxygen in the room. The strategy being employed here is to rapidly increase the background level of GI immunity in the local population to interrupt the chain of transmission. Since last year, the response to outbreaks of cVDPV2 is to give out the new nOPV2, and it is an improvement from a safety point of view. Unfortunately, just this month six cases of paralysis due to circulating nOPV2 have turned up in Africa—apparently related to two separate events of the virus mutating to a virulent form. How can we say the new vaccine is safer? 600,000,000 doses have been given out worldwide since it was adopted by the WHO, and far more cases than six would have been expected based on historical data for the old vaccine. The undeniable fact remains that we have now introduced another man made virus into human circulation, which for now at least, is very rarely causing disease.
I want to stress that the inactivated Polio vaccine used in the US and many developed nations never causes this problem and is incredibly effective. The reasons for persistence of the oral vaccine around the world are primarily related to cost, and ease of administration in remote isolated areas. But what is the end game? It’s been 35 years since the WHO announced the plan to eradicate polio by the year 2000. I personally see little likelihood of success under the current circumstances using the oral vaccine. There are multiple factors: the oral vaccine has limited effectiveness in the very places where Polio still exists in the wild, because of very poor sanitary conditions there, exposure to Polio virus (whether natural or vaccine derived) is extremely high, thus overwhelming partial immunity, and violence against healthcare workers in vaccination programs is accelerating in the third world. The fact that vaccinated children can and do occasionally get Polio is not exactly a plus for vaccine enthusiasm. Vaccine hesitancy or rejection in the third world should be viewed through the lens of human nature, and not just dismissed as illogical and unscientific. 1952 was the peak year for Polio in the US and 60,000 children were paralyzed, and 3000 died. With those grim statistics as a backdrop, there was essentially no hesitancy when the first vaccine became available in 1955. Contrast that with the psychologic impact of being a parent in Africa or South America whose child is paralyzed by a vaccine given for a disease that has not existed on your continent during your lifetime. You can be sure that parent will speak to all their friends, family and village, and the Greater Good will not enter the conversation. Meanwhile the oral vaccine paralyzes many hundreds more children than the natural disease every year. First do no harm, should not be incompatible with the more Utilitarian approach of Public Health to create the maximal utility or good. The WHO and nation states need to accelerate the use of inactivated Polio vaccine, even a single dose given in a regimen of primary oral vaccination would protect many children from circulating oral vaccine disease.
Thanks for your time! I read today that a US University has developed a computer algorithm which accurately identifies scientific material written by ChatGPT 90% of the time. That’s good, we want to keep people from pretending that AI generated material is their own. The only exception I can see might be in Washington DC where any injection of intelligence would be a welcome change.