The Big Disconnect
I understood that Biden proclaiming the “Pandemic is over” just before the midterm elections was a well timed political utterance, nothing out of the ordinary. How much it influenced people’s behavior is debatable, and likely to breakdown strictly along party lines. Now however, we have reached a real milestone with Saturday Night Live presenting a lengthly skit making fun of getting COVID, as a way of snatching an extra ten days vacation from work and general life responsibilities. The skit debuts the Always Positive rapid test to show your boss. It seems that the folks who were the most consistent about COVID mitigation strategies, including the crowd who were hypercritical of, “deniers and self-centered people risking other people’s lives”, suddenly decided, somewhere between Halloween and Thanksgiving, that they had had enough—and what better validation can you get than Saturday Night Live? The reality on the ground here in the US, and around the world, is that there is no significant improvement in the last several months, in fact another, new variant driven winter wave of COVID is sweeping the world, coinciding with a severe early Influenza season and continued high morbidity from RSV. I’m no psychologist but my take home is that people have very different tolerances for major social, lifestyle changes and discomforts, and that almost everybody eventually finds their limit. Let’s look at some data now.
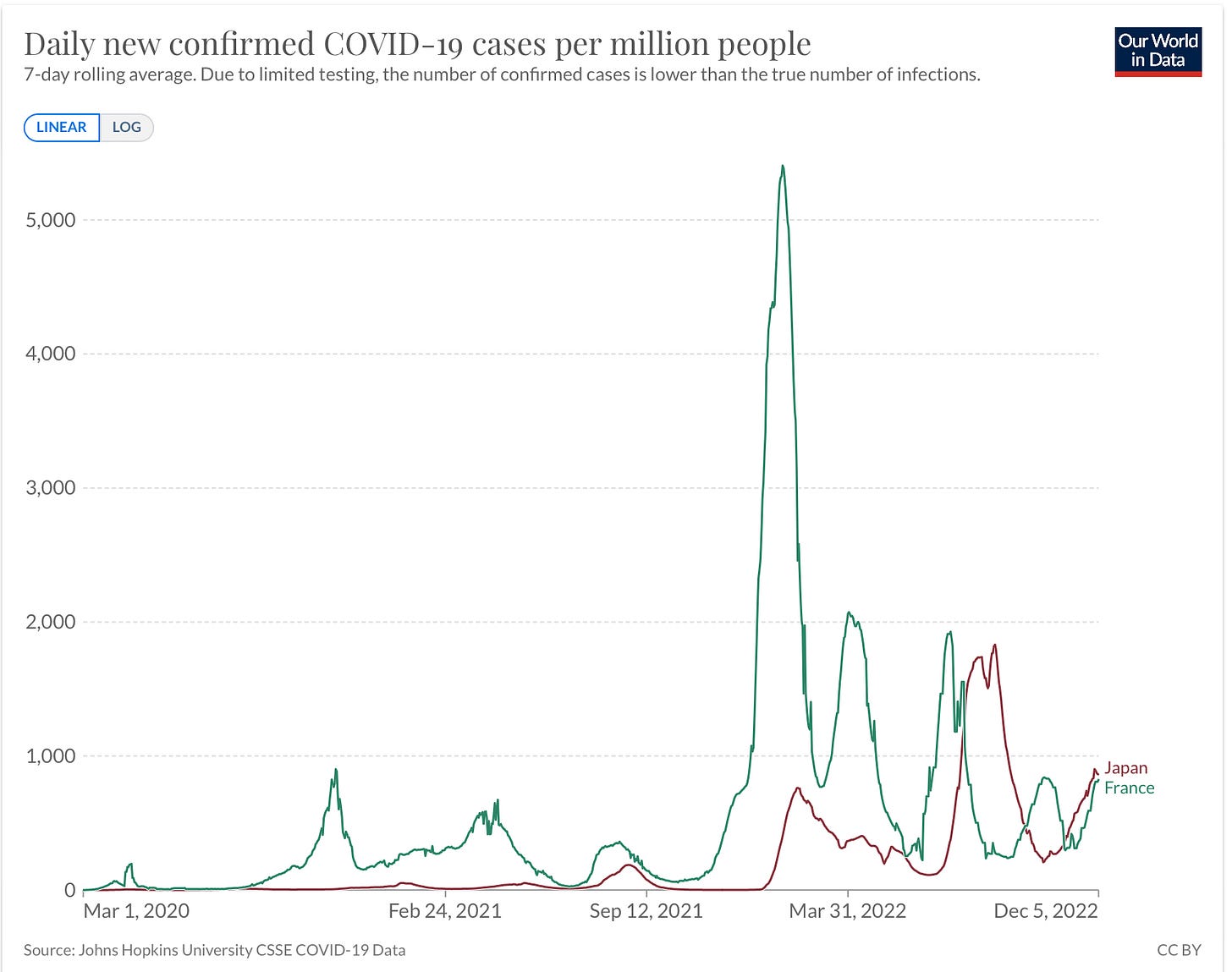
Several posts ago I mentioned that declining cases in France, which was very early into the COVID winter wave, looked quite favorable for what we might experience— not withstanding the fact that France has higher booster penetration that the US. The following graph shows that unfortunately France is on the upswing again in both cases and hospitalizations. As of last Friday the moving average of cases was 54,000, more than double the number in early November. Japan is following an almost identical trajectory with rapidly escalating cases. It’s not clear at this point, but suggestive, that the recent dominance of BQ.1.1, which is more immune evasive than BQ.1, is driving the renewed French wave.
Here at home there is nothing to suggest the situation warrants the dramatic change in behavior we all sense; psychologic factors appear to be the driving force rather than a logical appraisal of the facts. The following graph of weekly new COVID admissions shows another steep ramp up, and past experience tells us that this will very likely continue too worsen into January. Deaths, an undeniable corollary of hospitalizations, are also showing the steepest rise since early last summer, when BA.4/.5 swept the country. This past week we reached almost 3,000 deaths, after spending several months in the 1900-2200 range.
Did the need to help protect the vulnerable suddenly disappear, perhaps with the advent of the new bivalent boosters? I would say, “Not in the least”. This past week saw the long predicted, variant mandated, retiring of the last available therapeutic monoclonal antibody, bebtelovimab, with no replacements on the horizon. As you know, we have an enormous population of immunocompromised individuals who can take all the vaccines and boosters thrown at them, but don’t respond with normal levels of antibody production, and who continue to be at increased risk for severe disease. Paxlovid remains an import therapeutic option, but let’s not forget that a 5 day course of Paxlovid only decreases viral production until your immune system has ramped up to help finish the job. Paxlovid rebound (much exaggerated in importance as we have discussed) confirms that the drug does not totally eliminate the virus in many or perhaps almost all people. An adequate immune response, or a dose of monoclonal antibody is important to finish the job. 90% of the 3,000 people dying last week were over the age of 65 (some with immune compromising diseases in addition to age) and it’s a good bet that many of the other younger people were immune compromised. The situation is further complicated by the relatively low prescribing rates for Paxlovid for people at risk, who should get it. Hardly a week goes by that I don’t get a call from some one telling me that they, or a close family member, has COVID, and without apparent contraindication, their physician would not prescribe the drug or prescribed molnupiravir—a vastly inferior drug, but easier to deal with for the physician. The California Department of Public Health just issued a bulletin to practitioners in the state, urging them to increase their prescribing of Paxlovid. Under therapeutic options for COVID in high risk people, the bulletin does not even list molnupiravir! The NIH COVID Treatment Guidelines list Paxlovid as preferred with an A-high level of confidence rating, and the other drug only as an option when the first choice is contraindicated, and with a C-low level of confidence rating.
Moving on to the Pet Peeves Department, we have an article generating a lot of buzz, published in the Annals of Internal Medicine, comparing surgical masks to N95 fit tested respirators in health care workers.
Medical Masks Versus N95 Respirators For the Prevention of COVID-19 Among Health Care Workers. Annals of Internal Medicine 29 November 2022.Medical Masks
This was designed as a non-inferiority study, and their conclusion was the results ruled out even a doubling of risk of acquiring COVID with surgical masks. I’m going to put it as tactfully as I can, “this is garbage science”. The author’s Study Limitations section should have been renamed, Why We Should Never Have Done This Study. The only thing I think one might conclude is that health care workers in Canada likely wear their N95 masks more reliably than in Pakistan and Egypt (where it’s a bit warmer). This study, partially funded by the WHO, has been roundly criticized by several experts, and a concise overall assessment is the following.
“There is no point continuing to run underpowered, poorly designed studies that are designed to confirm existing biases,” Raina MacIntyre, PhD, professor of global biosecurity and head of the Biosecurity Program at the Kirby Institute, in Australia.
Next up is the very disturbing occurrence of a large measles outbreak in Ohio, which has sickened at least 60 children in multiple counties so far. None of the children are fully vaccinated, although 3 had received their first measles vaccine. Unlike COVID or Influenza, Measles vaccine is incredibly effective at preventing infection in people immunized with 2 doses. Unlike COVID, Measles has a very high morbidity rate in the young—23 of the 60 children were hospitalized, and we don’t like to admit cases of extremely contagious diseases to the hospital unless they absolutely require it. It seems likely to me that many people born into the MMR vaccine era simply don’t have any real conception of how severe, and potentially lethal this disease is. The WHO reports that at least 140,000 children died from Measles in 2018, the last year for which we have full data, and that in the period from 2000-2018 vaccination reduced measles deaths by 73%, or approximately 23.2 million lives saved—pretty good bang for your health care buck, not much even comes close. The WHO also estimates that 40 million children around the world missed their first measles inoculation as a result of COVID lockdowns and other Pandemic interruptions. That is a pretty large iceberg on the horizon. London officials reports that only 75% of children in the city have received their first Measles vaccine on time, and there are districts in the city where the rate is 60% or lower. Although this vaccine is incredibly effective at 98%, because of the extreme contagiousness of Measles it is necessary to vaccinate 95% of the population to prevent community spread and large outbreaks.
On the subject of vaccines and boosters, here is a huge population study from Norway looking at the COVID vaccine boosters during the early Omicron era. Turns out Norwegians are not much different from Americans—aside from missing a seat on the diversity bus and having a penchant for hiking.
Effectiveness of mRNA Booster Vaccination Against Mild, Moderate and Severe COVID-19, Caused by Omicron Variant in a Large Norwegian Population Based Cohort. Journal of the Infectious Diseasees, Volume 226, Issue 11, Dec. 2022, Pages 1924-1933.
The study compared the added benefit of a booster dose to people with the 2 dose basic regimen. Results are not surprising, showing much better performance of the booster in preventing moderate and severe disease, and virtually no effect on mild disease, even shortly after the booster, with zero effect on mild disease by 120 days. The graph below gives a concise view of the results. The booster efficacy in preventing severe disease was 81% for the first month and had fallen to 63.4% by 90 days. There also is a reduction in efficacy based on age, with the over 60 yo group faring even worse with regard to prevention of severe disease, but the confidence intervals for this group are large. (Is there any real surprise almost everyone dying now is over 65?)
Note the huge confidence interval for mild disease at 120 days, and please don’t let anyone convince you that the vaccine is CAUSING disease at that point. How do I sum this up? If you are at risk for severe disease, take the new booster and get several months of moderate protection from severe disease. Just remember, the effect is of intermediate efficacy, significantly diminishes over several months, and nobody will be offering you another booster at that point. We can hope that the new bivalent boosters do a bit better, but don’t count on any extra-base hits. So use your Clear and Present Thinking with regard to how you wish to safeguard your health.
It’s that time of the year when there is lots of talk about loving you fellow Human Beings—what an excellent suggestion, although I’m giving a pass to Vladimir Putin and his arms dealing friend. Use the like button up top if appropriate, for every 100 likes I promise to solve one pressing world problem of your choice.