This week Ghebreyesus, the Director General of the WHO, declared Monkeypox to be a Public Health Emergency of International Concern (PHEIC). This was an individual decision, made against the consensus of the expert panel convened to advise on the Monkeypox outbreak. The same panel had also advised against a declaration a month ago. There have been about 16,000 reported cases and a total of 3 deaths, all reported from Africa, and at least one of these was an immunocompromised individual. Why would anyone object to such a declaration? Doesn’t it make sense to act quickly, and put in motion efforts which might nip this epidemic in the bud and potentially stamp it out? The answer is simply one of priorities, and the relative risk of Monkeypox compared to any number of other pressing public health problems around the world competing for funding. The declaration of of a Global Health Emergency will unlock resources and undoubtedly divert them from other goals. I suppose it is understandable in light of the significant negative publicity the WHO has endured for what many have criticized as their belated designation of COVID as a Global Public Health Emergency, and then finally a Pandemic. A reasonable pragmatic approach is to ask how exactly you could stop transmission of this disease. You could convince people to stop having sex which would be low cost, but about as unlikely to succeed as eliminating COVID from the world scene. Alternatively you could attempt to vaccinate the vast majority of sexually active gay and bisexual men and their widening circle of partners, and that will take an enormous amount of resources and time. Also as I alluded to in an earlier post, the current vaccines were developed against a strain of the virus which is somewhat different from the current circulating strain, which has a different mode and level of transmissibility. We might just find out that the current vaccine decreases clinically apparent disease but does not reliably prevent infection. Wouldn’t that be a shocker! Allowed to spread unfettered, the Pox virus will have enormous opportunities to mutate and potentially improve its transmissibility, or up its virulence; so there are no easy answers. My guess is that the genie is out of the bottle, but luckily it causes incredibly mild disease so far.
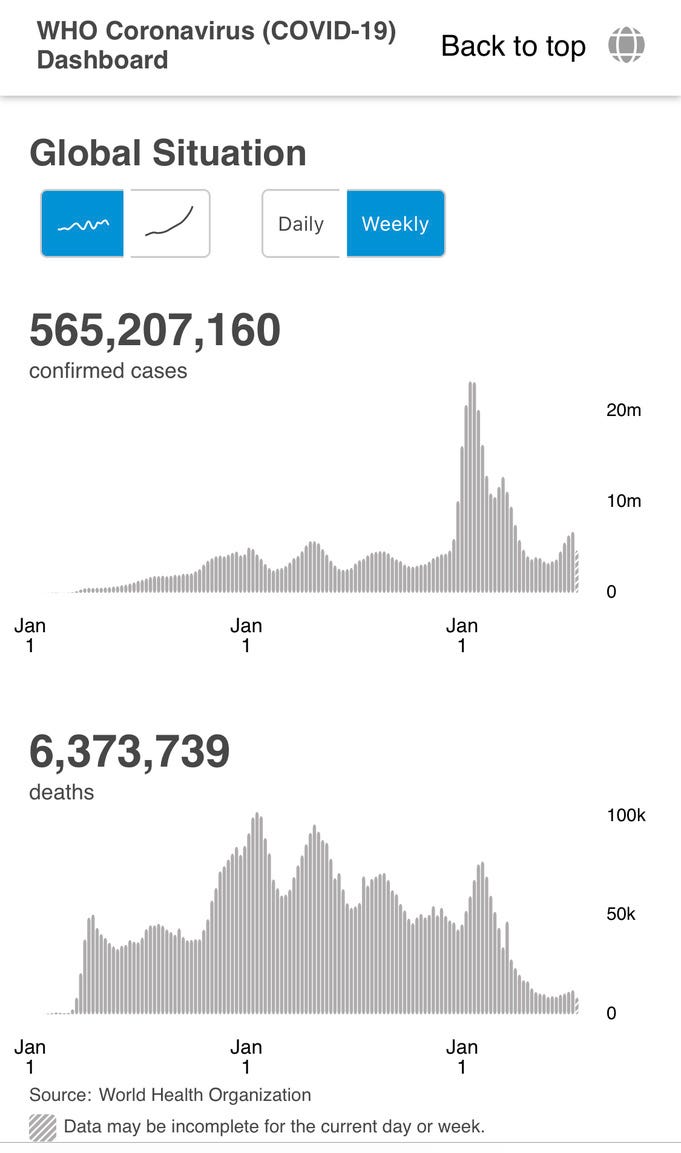
COVID cases around the world continue their spiral upwards, driven by the BA.4/.5 wave. Worldwide daily new cases have reached 1,100,000, with the real number being perhaps ten times that. That is a level second only to the Omicron winter wave, and if the true number were accurately known, perhaps surpassing that high water mark.
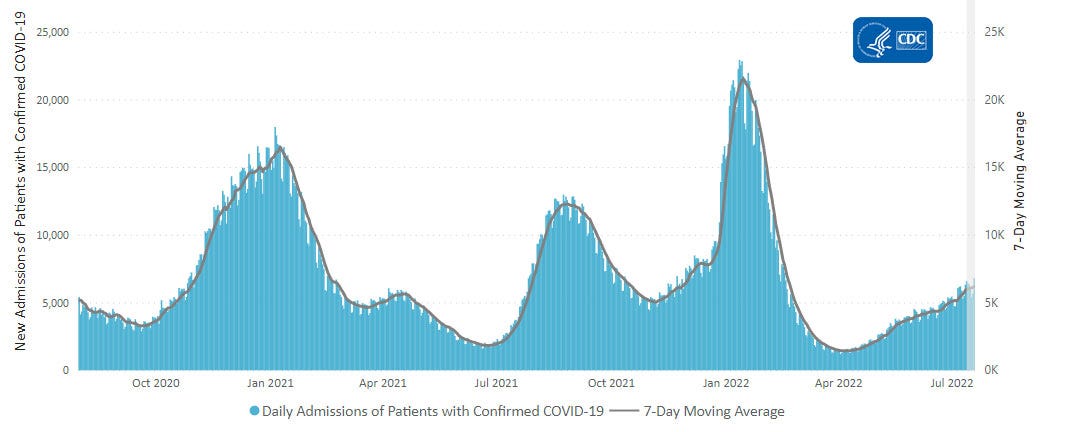
Since case counts are so unreliable, here is the CDC’s latest graph of daily hospitalizations in the US. As is apparent, there has been a steady unrelenting upward slope in the number of new daily hospital admissions, currently around 6500/day, since the end of April. As predicted, deaths are also rising although not at levels seen during the Omicron wave, and have increased from 200 to 350/day.
Our current vaccines are unable to prevent infection, particularly from BA.4/.5, and our current behavior reflects a sense of the inevitability of disease, and the exhaustion of patience with social mitigation practices. This combination is fueling the current massive wave infections. Joe Biden coming down with COVID was the culmination of a steady parade of our most ardent governmental mask and vaccine enforcers succumbing to infection. Loose the fist bump, not the mask is perhaps the lesson for anyone taking notes. BA.4/.5 has continued its push to soon become essentially the only circulating COVID variant as shown in the following CDC Nowcast graphic. This is the most transmissible, immune evading iteration of the virus to date. Luckily the portion of our immune systems referred to as T-cell immunity has remained relatively resistant to the evolutionary march of the virus. This arm of the immune system is slower to come into action than neutralizing antibodies or the Interferon mediated portion (called innate immunity). It doesn’t prevent the virus from gaining a foothold, but it is critically important in limiting the severity of disease. Most importantly our T-cell immunity (whether vaccine or natural) has proven to be fairly adept at recognizing and responding effectively to a wide variety of the COVID variants, and also to have good staying power. It is impossible to accurately measure the rate of rise of new cases, but we are seeing a slower ramp up of hospitalizations than had been the case when earlier variants rose to dominance. Through a mounting combination of prior natural and vaccine related immunity, the younger and healthier portion of the population is largely avoiding hospitalization. Many high risk individuals have been culled by the five waves of disease over the last 2 1/2 years, so there are fewer targets the virus can send to the hospital, thus the rate of increase is slowed down.
In the last post I referenced BA.2.75 as a scariant only, but worth watching. The lack of rapid growth over the last 2 weeks in the US has me feeling more optimistic that this variant is unlikely to be the next big thing following BA.4./5. The situation in India appears to be fundamentally different, since they did not experience a massive wave of BA.4./.5 as we have. There is a complex set of circumstances determining whether a given variant will spread rapidly in different populations. Factors include the age and average immune competence of the population, the amount of vaccine and prior natural immunity, which variants have caused large waves of disease previously, and the timing of the introduction of the variant in relation to prior waves of disease and vaccine boosting. This is readily evident in the following graph showing new daily cases and COVID deaths in New Zealand throughout the Pandemic.
New Zealand was once highly touted as a model for containment of COVID, and very highly vaccinated with 85% of the entire population over age five fully vaccinated with either Pfizer or Astra-Zeneca vaccine. Held up by some as the opposite model of everything we in the US did wrong— New Zealand is now reeling under the highest daily case counts, hospitalizations and deaths of the entire Pandemic. They currently have the highest reported death rate per capita in the world. The only reasonable explanation I can see between the severity of BA.4/.5 in the US and New Zealand is the prior immunity built up here as result of wide spread infection with previous variants. Various political leaders might have thought they won the game by shutting down their societies for long enough to confront a less severe form of the virus. You can run, but apparently you can’t hide forever from the sons of Omicron. Attempts to judge the severity of a given variant at this point in time are highly limited by so many complex variables as to be basically useless.
Finally on the Friendly Advice Page today we have the following. If you are contemplating going to a wedding, or similar indoor event, where you will be spending significant time without a KN95 mask, then do it with the expectation that there is a high probability you may get infected. That includes people who have been vaccinated and boosted or double boosted, and those with histories of prior COVID infections, even multiple times. Reinfections are at the highest level since the start of the Pandemic, and even infection with the original Omicron BA.1 is not reliably protective in the face of BA.4/.5. Factor into your risk reward calculation, your age and underlying immune competence, or severe underlying medical disease, which could make you a candidate for more serious disease.
Thanks to everyone interested in these pages. Subscribe if you haven’t already and share with friends, family and colleagues.





what to advise 70+ year old with comorbidity who is relatively well?
what about restaurant ,small group meetings , are important .
what mask .
although many have been posted twice ,I think that may not be enough
Frank Forte